Challenges to Improving Diagnostic Accuracy – Part 1
Clinical Case:
A young toddler with fever and fussiness presents to the urgent care. History reveals she has had upper respiratory symptoms for three days and is occasionally pulling at her right ear. Her exam is remarkable only for clear rhinorrhea and partially visible right tympanic membrane (see image below). Attempts are made to remove cerumen, but views of the TM are not appreciably improved. The mother is concerned that her child has an ear infection and questions whether or not she needs antibiotics. What should the clinician do in this situation?

The Challenges:
The number of investigations undertaken to answer this question is impressive. We all know the rationale for these efforts—acute otitis media (AOM) is common but antibiotic use needs to be judicious for the good of both the individual and public. Yet despite the sheer number of person-hours invested, there still remains variability in practice among clinicians when it comes to diagnosing AOM and other middle ear conditions, most notably otitis media with effusion (OME). The reason for this diagnostic confusion likely stems from three interrelated challenges:
1. There is often difficulty in obtaining an adequate view of the tympanic membrane (TM). Otitis media is a physical diagnosis but, as in the case above, the target of our assessment is frequently obscured or not easily accessible. This incomplete (often) and fleeting (almost always) view of the TM is certainly one of the root causes for the widespread inconsistencies and lack of otoscopic competency.
2. Like many pathologic conditions, AOM and its variety of signs and symptoms does not have a defined start and stop. On the contrary, AOM develops and resolves in a progression, thus signs and symptoms will also demonstrate progression (ex. mild, moderate, severe bulging). Others have defined these transitional states–aptly termed transitional otitis media–as representing a progression in either direction from AOM to OME. Furthermore, the 2013 American Academy of Pediatrics practice guideline recognizes that this impacts the certainty of diagnosis. Thus, compounding the challenge of visualizing the TM, is the need to interpret the continuum of various physical findings and determine which warrant antibiotic therapy, when to “watch and wait”, and when to avoid antibiotics.
3. Otoscopy training is limited. Even if a program does offer a formal curriculum, the majority of education still occurs at bedside where the trainee and attending physician compare findings. In traditional otoscopy, slight variations in technique greatly impact the degree of visualization of the TM. Thus, it is common for a trainee’s view to differ from that obtained by a more experienced clinician, contributing to confusion about what findings may (or may not) have been present. Clearly this comparison of exams is an inefficient approach to impart competency in otoscopy.
A Novel Solution:
Over the years, many individuals have significantly advanced our understanding of AOM. Thanks to their efforts, we know what physical signs are important (more on that in Part 2), the pathogens to consider, what treatment strategies work best, and even how to decrease risk in young infants. Yet the above challenges remain because the devices traditionally used to visualize the TM are not significantly different from those utilized in the 1800’s. Simply put, until recently, otoscope technology had not evolved in a manner to provide clinicians with the best tool to address the diagnostic challenges. This technology gap is finally being filled by digital otoscopy. While expensive and bulky digital video endoscopes have been used by ENT specialists for some time, recent advances have made it suitable for everyday office use. Devices such as the Wispr offer the clinician a tool that allows her to quickly obtain an image or video of the TM, take her time while evaluating the image for signs of pathology, and use the images to teach, learn and disseminate competency.
Case Resolution:
As luck would have it, another provider had brought his Wispr otoscope to work and offered to re-examine the child. The following image was obtained after advancing past the obstructing cerumen.
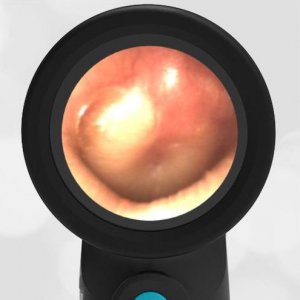
Acute Otitis Media (AOM)
As can be seen from the image, a certain diagnosis of AOM based on a severely bulging TM could be reached. With the enhanced view, a knowledge of the important physical signs, and the ability to share and learn from clinical images, correctly diagnosing and managing middle ear conditions becomes much easier. And as the use of digital otoscopy spreads, the cumulative impact will be a leap forward in diagnostic accuracy, improved patient care, and antimicrobial stewardship.
Coming Soon: “Seeing is Believing Part 2“, where we will take an evidence-based look at physical findings associated with AOM.

