One of the most common reasons for a pediatric visit to urgent care or the emergency department is an ear complaint. Traditional otoscopes are challenged by being able to obtain a diagnostic image in a small, partially occluded ear canal in a squirming patient. In addition, a traditional otoscope does not have have the ability to document the exam and track for changes. In this article WiscMed presents an imaging study using the Wispr otoscope spanning from the initial diagnosis of acute otitis media (AOM) to it’s resolution. Key features of each image are annotated and described.
The case
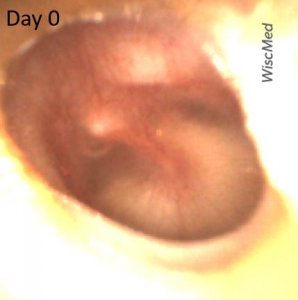
An 18-month-old female is brought into the emergency department (ED) with concerns for vomiting, fever and fussiness. The child had historically been well and is age-appropriate vaccinated. The symptoms began 2 days earlier. Symptoms initially included pulling at the ears, escalating to vomiting, poor feeding and fever to 103 F. The parents treated with antipyretics but became concerned when the child seemed to be declining further. They brought her to the ED with a primary concern of dehydration. In the ED, she was found to have brisk capillary refill, elevated heart rate and a fever of 102 F. Influenza and COVID tests were both negative. Urinalysis was also negative. The following image of her left ear was obtained.
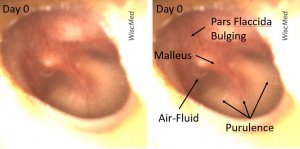
Day 0 left ear exam – does not meet criteria for acute otitis media (AOM)
The day 0 exam reveals a tympanic membrane (TM) that is clearly not normal. There is bulging of the pars flaccida, an air-fluid level and purulence in the middle ear space. The presence of the air-fluid level, and the lack of bulging of the pars tensa suggests that this currently represents a middle ear effusion (MEE) with a functioning Eustachian tube. In consultation with the mother, antibiotics were not initiated at this visit.
The mother returned with the child the next day. The child continued to have a fever, vomiting and diminished wet diapers. A repeat exam of the left ear revealed the following.
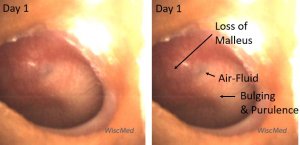
Day 1 left ear exam – meets criteria for AOM
The pathology in the left ear has evolved since day 0. Now, there is loss of the malleus bony landmark, bulging of the pars tensa and scant air-fluid. The remaining air-fluid is likely trapped and not an indication of a functioning Eustachian tube. This image meets the diagnostic criteria for acute otitis media. The child was started on antibiotic therapy.
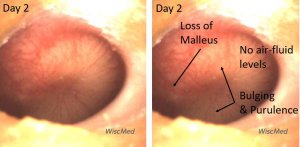
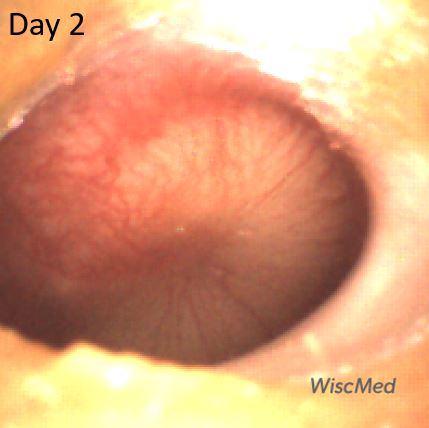
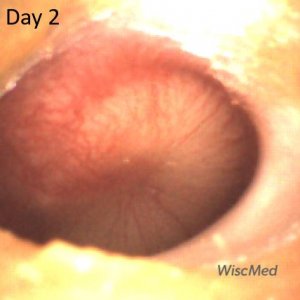
Day 2 left ear exam – child had received one dose of antibiotics
The day 2 exam is perhaps slightly worse than the day 1 exam. At this time, the child had taken one dose of antibiotics. There continues to be bulging, erythema and loss of bony landmarks. In addition, the air-fluid level is gone confirming that the Eustachian tube is not venting the middle ear space to the posterior nasopharynx.
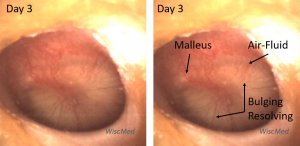
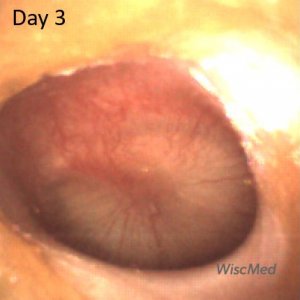
Day 3 left ear exam – mild improvement
The day 3 left ear exam is notably improved. The child has had 3 doses of antibiotic. The bulging of the pars tensa is resolving, the short process of the malleus is discernable and there is once again an air-fluid level. Clinically, the child looked much better at this visit. The mother reported that her fever had resolved and that she was eating and drinking with more enthusiasm.
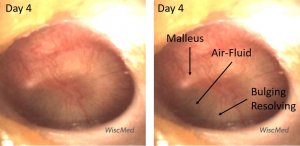
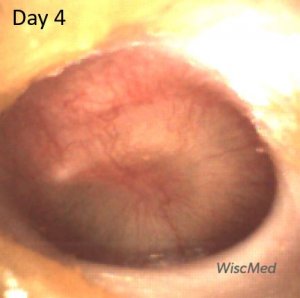
Day 4 left ear exam – continued improvement
On the day 4 exam, the air-fluid level is more apparent. Pars tensa (PT) bulging continues to improve.
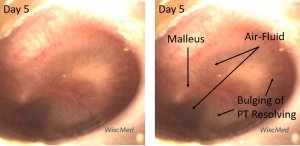
Day 5 left ear exam – continued improvement
On the day 5 exam, the purulence behind the TM is resolving.
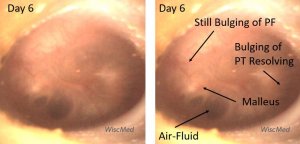
Day 6 left ear exam – presence of air-fluid bubbles
On the day 6 exam, air-fluid bubbles are clearly present. The bulging of the pars tensa has almost completely resolved. There is still bulging of the pars flaccida (PF). The short process of the malleus is discernable, but the remainder of the ossicle is indistinct.
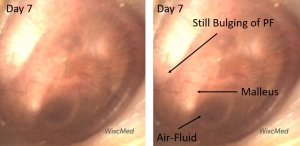
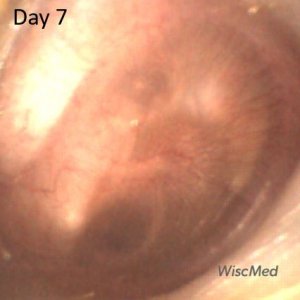
Day 7 exam – similar to day 6
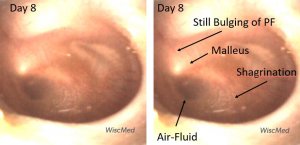
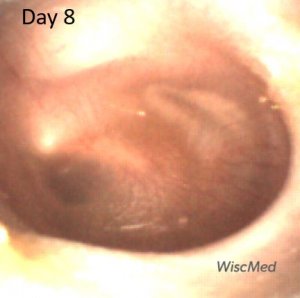
Day 8 exam – shagrination developing
The day 8 exam shows a feature often found in resolving AOM. Shagrination (cobble stoning) of the tympanic membrane occurs as the bulging of the TM subsides. Shagrination might be thought of as “tympanic membrane stretch marks.”
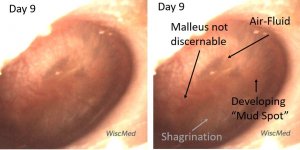
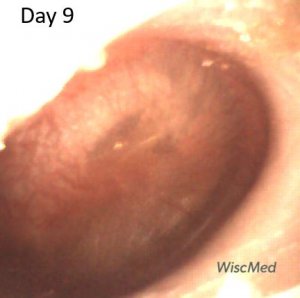
Day 9 exam – emergence of a “mud spot”
The day 9 exam shows another feature commonly found in resolving AOM. Mud spots are well described in Chapter 9 of Dr. Michael Poole’s excellent book, “Otitis: The Expert’s Diagnostic Guide.” Mud spots are often found in cases of resolving acute otitis media. They are typically seen from one to eight weeks after AOM and are located on the medial surface (middle ear surface) of the TM. Mud spots are thought to be from aggregation of inflammatory cells secondary to the resolving infection. The spots resolve with time as can be seen in the panels below. The mud spots appear to resolve more quickly if there is no middle ear effusion present. Dr. Poole has introduced the term Resolving Middle Ear Muco-Purulence (REMEMP) as a more academic term than “mud spots.”
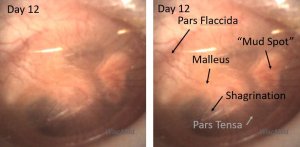
Day 12 left ear exam – prominent mud spot
On the day 12 exam, the pars flaccida is still mildly bulging, shagrination is present and the mud spot has organized and coalesced.
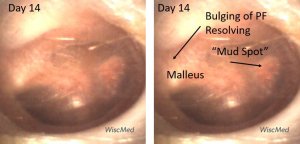
Day 14 left ear exam – mud spot resolving
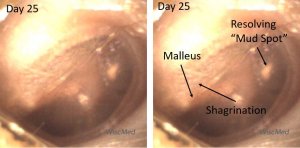
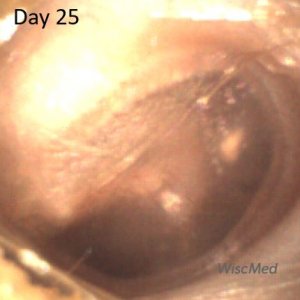
Day 25 – shagrination of the pars flaccida
On the day 25 exam, the left ear has almost returned to normal. The mud spot has mostly resolved. Erythema is gone. Most of the malleus is discernable. The shagrination of the pars flaccida suggests that the bulging in this area of the TM is also resolving.
Here are the daily exams in sequential order.





The videos and images from the daily exams for this case are available here for download. WiscMed requests attribution if these are used in a presentation.
James Berbee, MD
Founder, WiscMed