Middle Ear Effusion
A 4-year-old girl is transferred to the Emergency Department (ED) from Urgent Care (UC) due to concern for hemotympanum (blood behind eardrum) after a fall. Shortly before arrival, the child was climbing on playground equipment when she fell from approximately five feet and struck her face on the ground. There was no loss of consciousness and she cried immediately. The parents noted swelling and bruising around her nose.
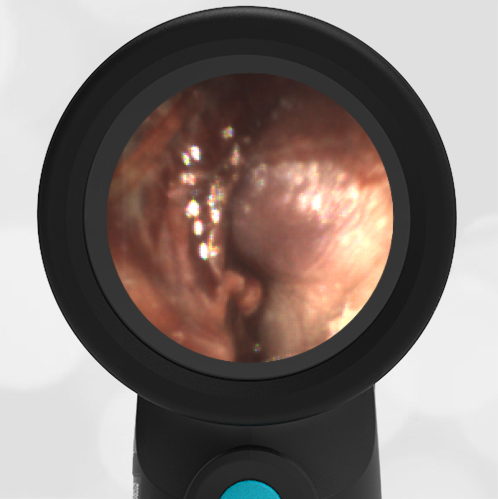
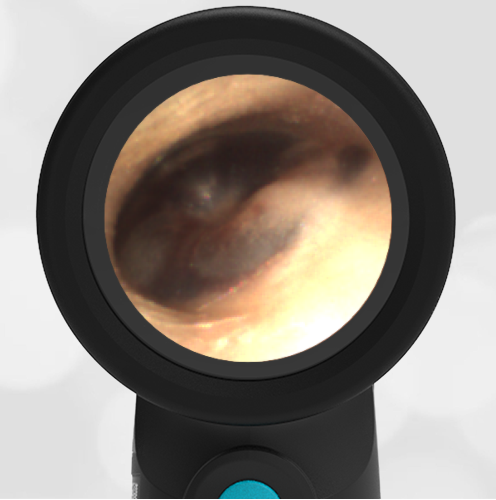
She was taken to an UC where the medical provider noted that the left TM appeared very dark, raising his concern for a hemotympanum and basilar skull fracture. Since the child appeared otherwise well to the parents, they declined EMS transport and brought her to the ED via private vehicle. Upon arrival, the child was well-appearing with an exam notable for mild swelling and bruising to the upper nose. There was no nasal septal hematoma, but a moderate amount of blood was noted in the left nare. She had no scalp hematoma nor any midface, orbital, or dental injury. The following image of her left ear was obtained with a Wispr digital otoscope.
Which of the following is the most appropriate course of action based on physical exam and Wispr findings?
- Emergent head CT
- Emergent Neurosurgical consultation
- Emergent Maxillofacial CT
- Observation, reassurance, and outpatient follow-up as needed
The correct answer is “4” – Observation, reassurance, and outpatient follow-up as required.
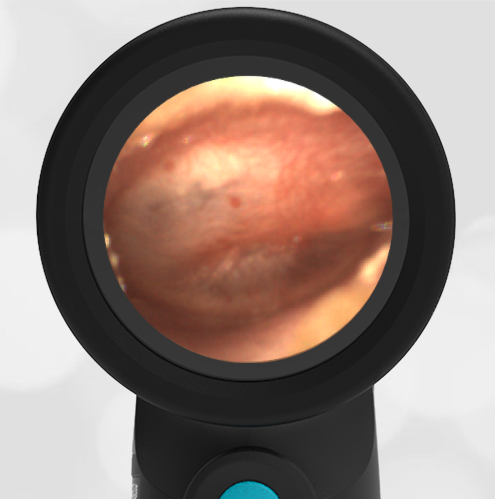
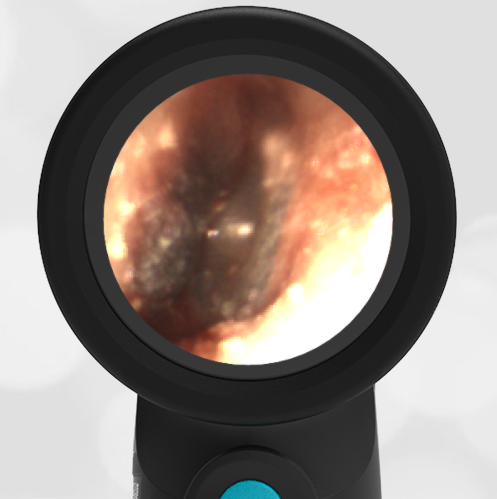
- Middle Ear Effusion – Left Ear
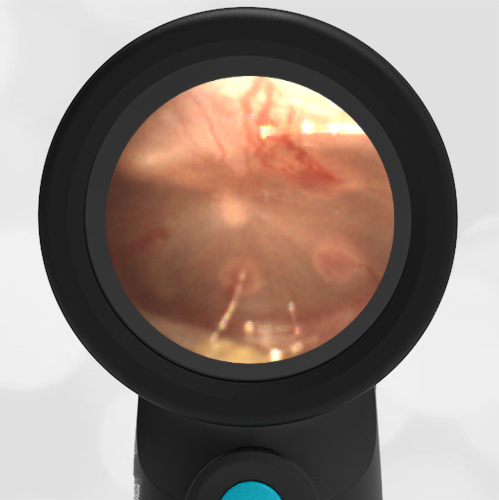
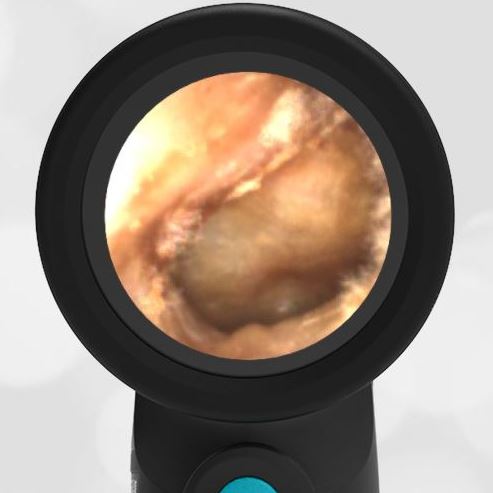
- Normal Ear – Right Ear
Based on the Wispr exam, the initial concern for the hemotympanum is equivocal. The left ear has a middle ear effusion (MEE) and the fluid appears slightly darker than expected for MEE. It is unclear if this was the finding noted at the UC since it is pretty subtle and the “very dark TM” report is not supported by the Wispr images. Based on the child’s overall appearance and reassuring physical exam, it’s most likely the child has a middle ear effusion from a prior undocumented infection. A diagnosis of hemotympanum is less certain. As observed in a more severe case of epistaxis, blood from the nasopharynx may enter the middle ear via retrograde flow down the Eustachian tube. It is also notable that the TM of this patient is not bulging, unlike the previous WiscMed cases of hemotympanum associated with basilar skull fractures. Thus, the best answer based on physical exam and Wispr findings is observation, reassurance, and outpatient follow-up as needed with ENT after nasal swelling subsides.
The child was observed in the ED for an additional two hours, did not develop any worrisome symptoms, and was discharged home with relieved parents.
Here are the left ear and right ear video exams:
|
Left Ear |
Right Ear |