Middle Ear Effusion – November 30, 2023
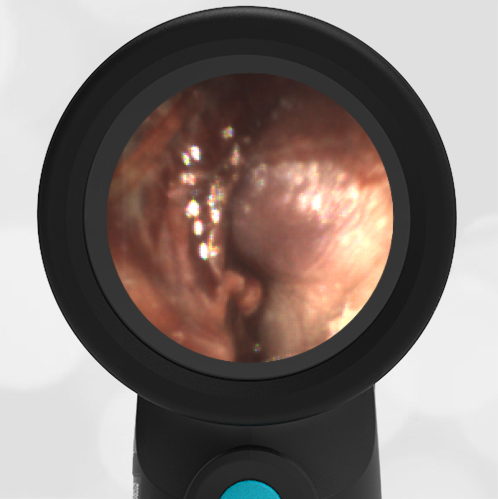
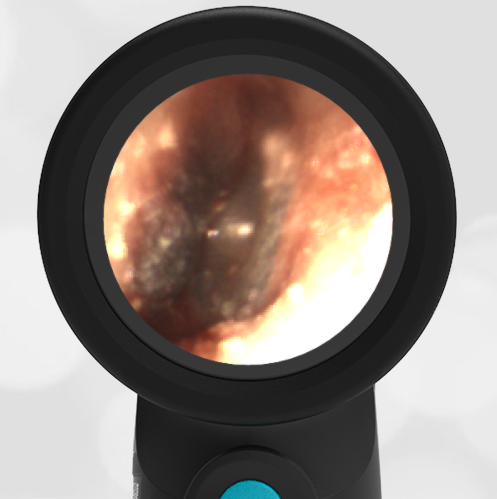
A 4-year-old child is brought to the emergency department (ED) for evaluation of a bloody nose (epistaxis). His parents note he gets them frequently, but this one did not stop with pressure “like it usually does.” The child has been congested for several days but has not had a fever and denies ear pain. His exam demonstrated a small amount of dried blood crusting the right anterior nasal septum. The child’s Wispr exam of his right ear is shown. The remainder of his exam is unremarkable.
What is the appropriate evaluation and management for this child’s condition?
- He has a middle ear effusion.
- He has mild bulging of the tympanic membrane (TM) and should be given a prescription for antibiotics to fill if needed.
- He has severe bulging of the TM and should be offered immediate treatment with antibiotics.
- The child has hemotympanum, from retrograde nose blood via the Eustachian tube.
Answer: A. He has a middle ear effusion.
This child has a purulent appearing middle ear effusion (MEE), an incidental finding to the presenting concern of a nose bleed. The initial inclination may be to start treatment for acute otitis media (AOM). However, it is important to not only determine if the findings are sufficient to diagnose AOM, but also if the symptoms are severe enough to warrant immediate treatment with antibiotics.
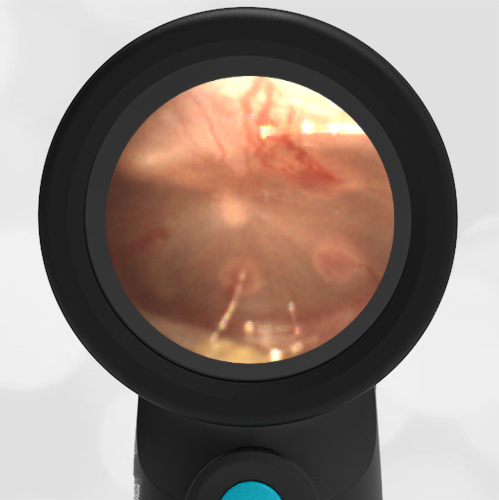
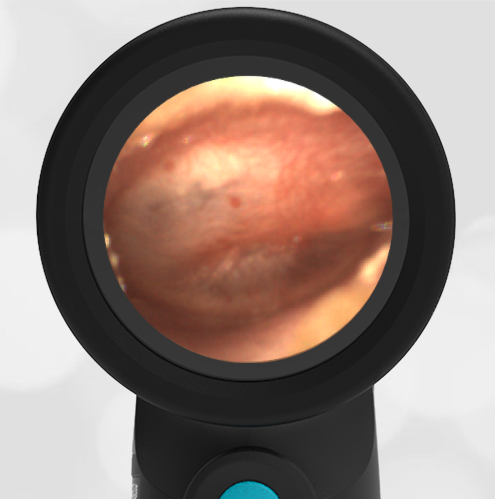
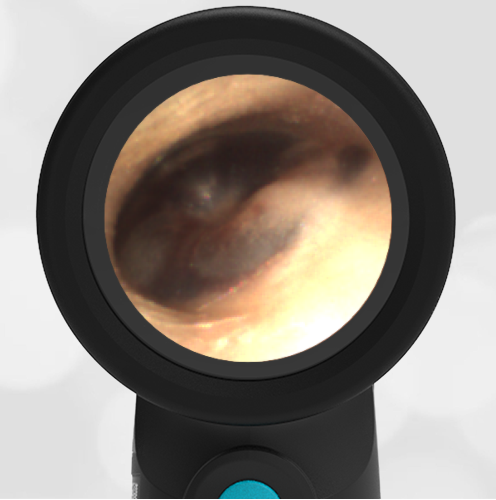
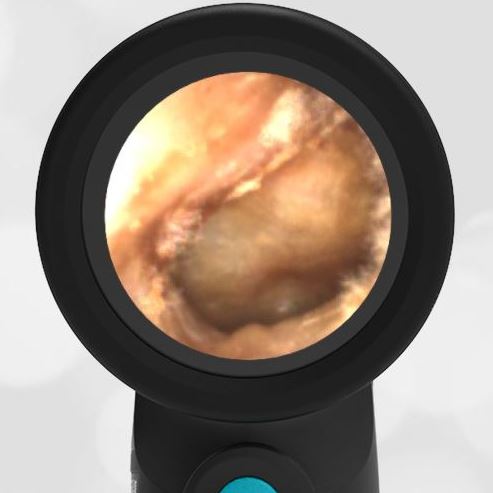
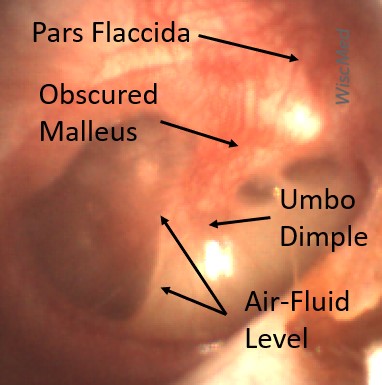
Research strongly supports using tympanic membrane (TM) bulging as a sensitive indicator of AOM. However, since bulging occurs on a continuum, clinicians must be adept at identifying mild bulging from moderate/severe bulging in order to make a confident diagnosis. The superiorly located pars flaccida is the most compliant portion of the TM and therefore is typically the first area to bulge when pressure increases in the middle ear space. With this early bulging, clear visualization of the bony malleus is impaired and the TM appears “full” with a slight umbo dimple located centrally. As bulging progresses, the central dimple becomes deeper and the malleus more difficult to visualize. With moderate to severe bulging, the deepening dimple results in the appearance of an “angry donut.”
This child’s TM does not demonstrate the donut sign, however, the malleus is not clearly visualized and there is a slight central depression—consistent with mild bulging of the pars flaccida. While mild bulging may be a sign of early AOM, it is also observed with fever, crying, and resolving AOM. Therefore, additional signs or symptoms—either recent onset of ear pain or intense erythema–must be present to diagnose AOM confidently. While there is some injection of the TM, it is not enough to make a definitive diagnosis of AOM and begin immediately initiating antibiotics.
Further supporting the withholding of immediate antibiotics is the lack of symptoms—our patient had no ear pain or fever. It is important to note that once AOM is considered, the actual treatment approach is based on the severity of signs and symptoms. Thus if a diagnosis of AOM had indeed been made based on mild bulging and erythema, the severity would be considered mild. As a child older than 24 months with mild AOM, observation for progression with a delayed prescription would be appropriate.
There is no evidence of blood behind the ear drum (hemotympanum), although retrograde delivery of blood to the middle ear space from a nosebleed does occur as shown in this case.
WiscMed has published a handy acute otitis media treatment poster based on American Academy of Pediatric (AAP) guidelines that may be found here.
Here is the complete video exam.