Hemorrhagic Bullae
A first year Pediatric resident presents the case of a 7-year-old female brought to the emergency department (ED) with a chief complaint of ear pain. According to the child’s parents, the ear pain worsened to the point of waking the child. She was diagnosed with influenza earlier in the week but seemed to be doing better with only a mild cough. Her fevers had continued and were responsive to ibuprofen.
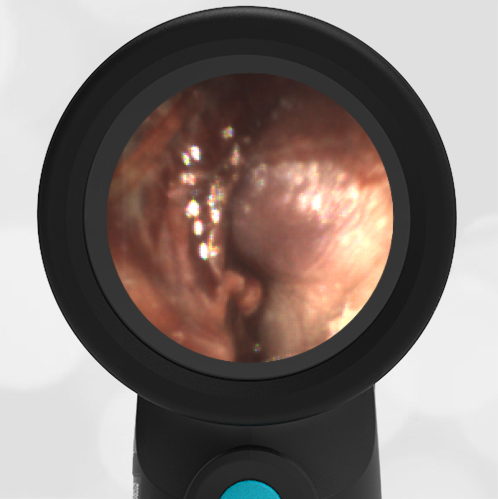
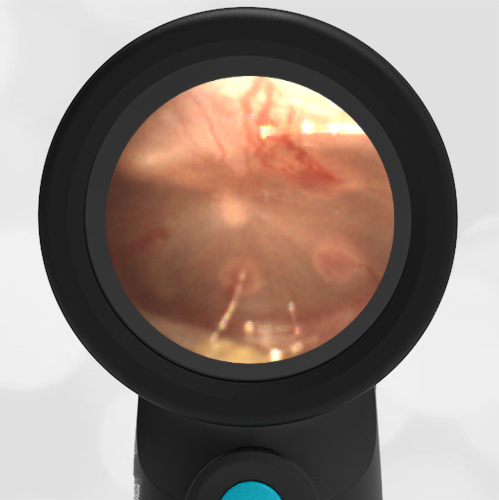
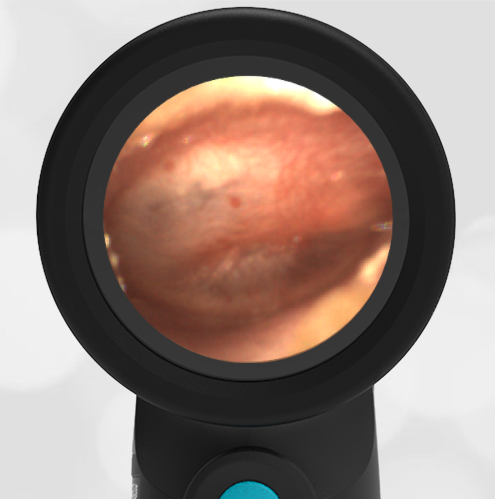
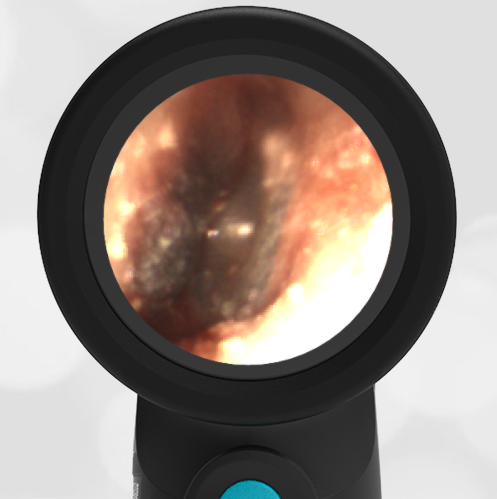
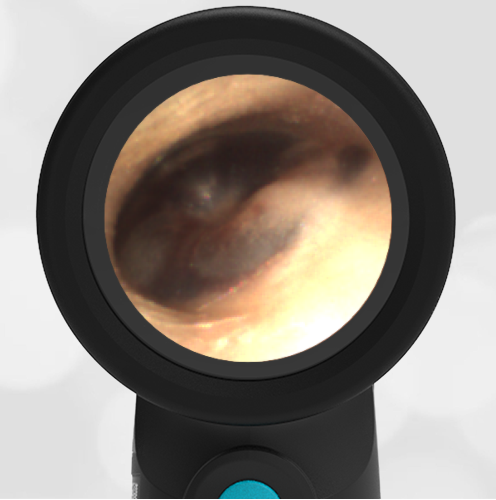
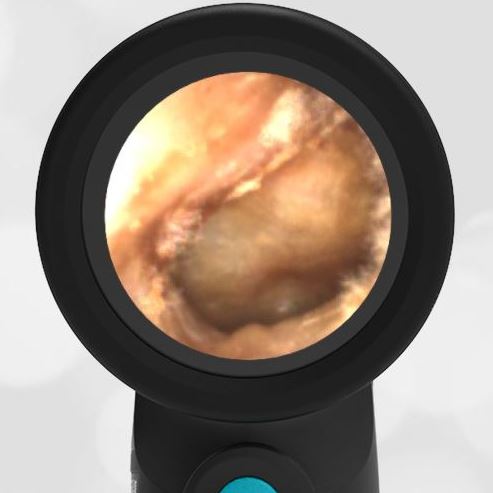
The child’s physical exam is unremarkable except for her left tympanic membrane (TM) which the resident displays on the Wispr otoscope for review. The resident summarizes her assessment of the patient as “I believe she has acute otitis media but I’m struggling to describe the findings.”
Does this child have acute otitis media (AOM)?
Yes, the child has AOM.
The resident can be forgiven for some uncertainty in describing his patient’s TM findings as there seems to be a lot going on and demonstrates why it is helpful to take a stepwise approach to our assessments. As described in Seeing is Believing Part 2, to determine whether a child has acute otitis media (AOM), begin with identifying the presence (or absence) of bulging. A few questions can help with this:
Does the TM look like a bagel/donut?
-If yes, then there is likely to be at least moderate bulging of the TM and a high likelihood of acute otitis media.
-If no, then we need to look at other landmarks and ask additional questions:
Can you clearly see the malleus?
-If yes, then the TM is not bulging and the likelihood of AOM is low.
–If no, then there is likely bulging in the pars flaccida (i.e. upper portion) of the TM, indicating at least mild bulging or “fullness” of the TM. This is not sufficient to diagnose AOM, so we need to ask an additional question:
Is there intense erythema of the TM? -or- Is the child demonstrating significant ear pain?
–If yes to either question, then there is a high likelihood of AOM.
–If no to either question, then then the likelihood of AOM is lower and antibiotics are not indicated.

When posed with these questions, the resident responded with: “No, the TM does not look like a donut. No, I cannot make out the malleus. Yes, the child’s TM has intense erythema and a lot of ear pain. I feel confident in the diagnosis of AOM.” Following this exchange, further bedside teaching allowed a more detailed level of analysis. The child’s TM appears to be developing a bullae consistent with bullous myringitis inferiorly and has a hemorrhagic bullae centrally. The resident endorsed being initially confused by these findings but reported a much greater degree of certainty in his ability to walk through the steps to accurately diagnose AOM. This is an advantage of the digital otoscopy that the Wispr provides.
Here is the complete video exam.
Complete exam video
Lieberthal A, Carroll E, Chonmaitree T et al. The Diagnosis and Management of Acute Otitis Media. Pediatric, Mar 2013; 131(3).
Rothman R, Owens T, Simel D. Does this Child Have Acute Otitis Media? JAMA, Sept 2003; 290(12):1633-1640.