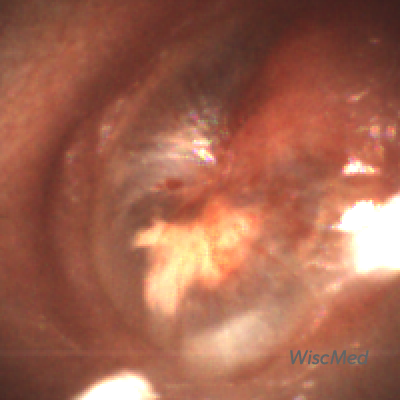
Mild Bulging AOM – April 27, 2023
A 7-year-old presents to the emergency department (ED) with right ear pain for one day. The pain started earlier in the evening and kept her awake, so her mom brought the child in for evaluation. Aside from ear pain, she has otherwise been well without fever, cough, or other respiratory complaints. The child has not been swimming recently and the mom does not report any ear drainage. Her mother states the child used to have frequent ear infections but has done much better since tubes were placed several years ago. Immediately prior to the examination, the child stated, “I just felt my ear pop and now the pain is better.”
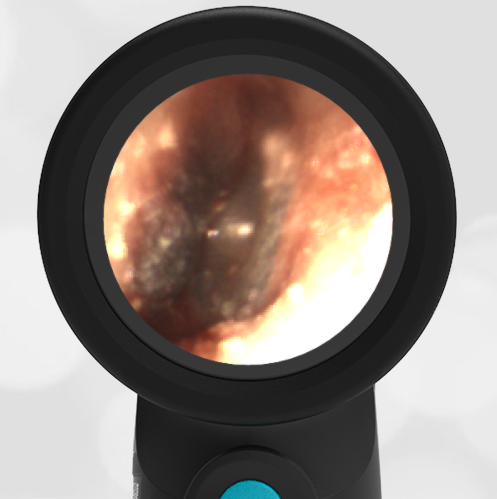
Her Wispr digital otoscope exam is shown.
Which of the following is true regarding this child’s presentation?
- The tympanic membrane (TM) is normal, and no antibiotics are indicated.
- The TM demonstrates a middle ear effusion (MEE), and no antibiotics are indicated.
- The TM demonstrates mild bulging and antibiotics may be prescribed “as needed” if symptoms worsen.
- The TM demonstrates severe bulging and immediate initiation of antibiotics is indicated.
The answer is 3, The TM demonstrates mild bulging and antibiotics may be prescribed “as needed” if symptoms worsen.
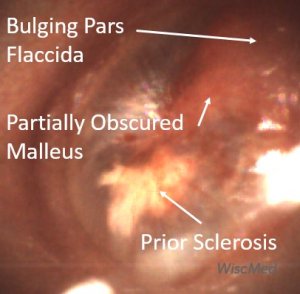
The child’s TM demonstrates mild bulging as evidenced by the bulging in the pars flaccida region that obscures the visualization of the malleus and distorts the normal light reflex. The TM has not progressed to severe bulging which would take on the appearance of a deeper central depression (i.e. donut sign). The child’s TM also has erythema, particularly centrally where small hemorrhages are noted. The white patch (sclerosis) noted in the posterior inferior quadrant is likely a result of her prior ventilation tube placement. According to the American Academy of Pediatrics (AAP) practice parameters for diagnosis and management of acute otitis media (AOM):
Clinicians should diagnose AOM in children who present with mild bulging of the TM and recent (less than 48 hours) onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal child) or intense erythema of the TM.
Given this definition as well as the child’s initial complaint of pain that brought her into the ED, one could argue for immediate initiation of antibiotics. However, given the child’s age (able to communicate clearly about her symptoms) and the improvement in her pain after her “ear popped” (suggesting her Eustachian tube opened and relieved some of the pressure), a reasonable course of action is to continue to address comfort and provide a “just in case” antibiotic prescription if her symptoms worsen over the next 48 hours. Despite pain relief and ear popping, there are no air-fluid levels present to suggest a middle ear effusion.
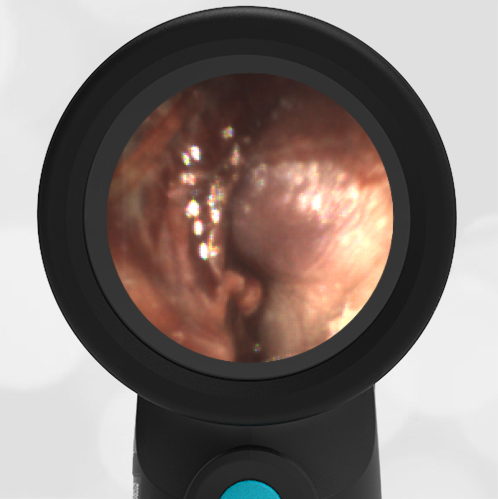
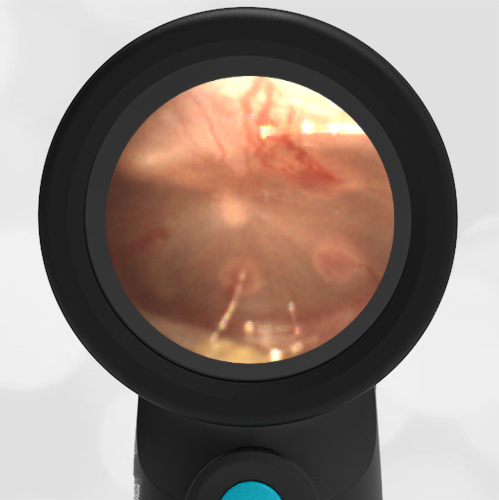
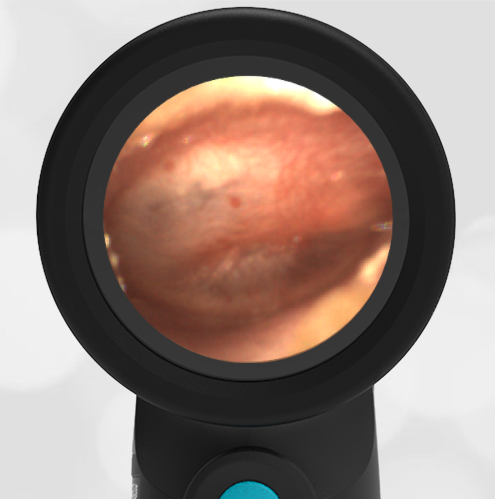
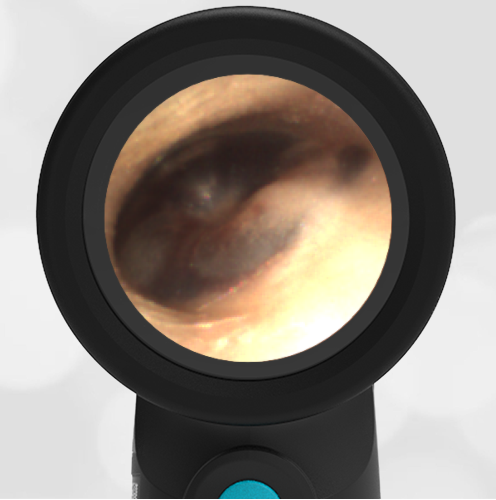
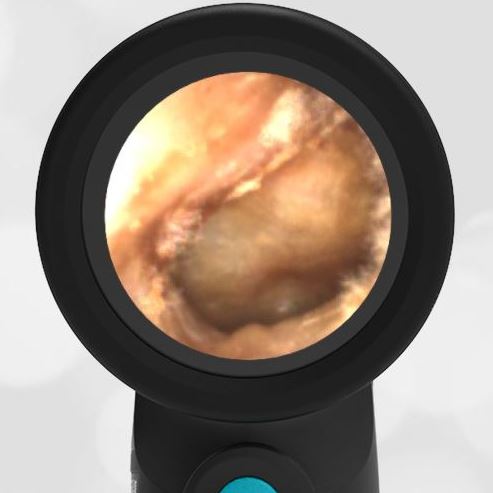
Here are examples of the ear conditions represented by the answer choices listed above.
- Normal Tympanic Membrane
- Middle Ear Effusion (MEE)
- Mild Bulging AOM
- Severe Bulging AOM
Watchful waiting management of acute uncomplicated AOM is supported by the AAP guideline. However, there appears to be resistance among clinicians to this approach as a recent review of the management of acute uncomplicated AOM demonstrated a high antibiotic prescription rate, particularly among non-otolaryngologists. The rationale for these differences remains to be determined, but uncertainty in diagnosis likely plays a role in the hesitancy of clinicians to defer antibiotic initiation. As can be observed in this child’s case, a very clear image of the TM allows conversation with the parent and provides confidence in the decision. After reviewing the images of her child’s TM, discussing how her child’s findings differ from that of certain AOM, and providing alternative strategies for management, the mother was very happy to defer antibiotics—while also feeling empowered to fill the prescription if the symptoms worsened.
WiscMed has created a visual diagnosis guide to common ear conditions that may be found here.
Here is the video of the complete ear exam:
Lieberthal A, Carroll E, Chonmaitree T et al. The Diagnosis and Management of Acute Otitis Media. Pediatric, Mar 2013; 131(3).
Slominski N et al. Watchful Waiting for Acute Otitis Media. Pediatrics (2022) 150 (1).