Middle Ear Effusion – May 18, 2023
A 10-month-old female presented to the emergency department (ED) with concern about an ear infection “that is not getting better”. She was seen two weeks ago and completed a course of antibiotics, but has continued to stick her fingers into both ears. Mom interprets this behavior as indicating pain and is worried because she has already been on antibiotics four times for ear infections.
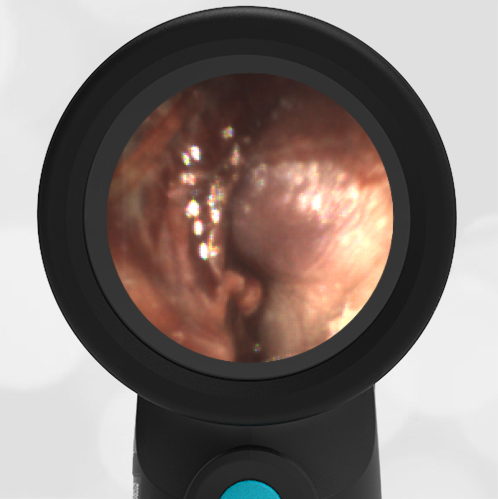
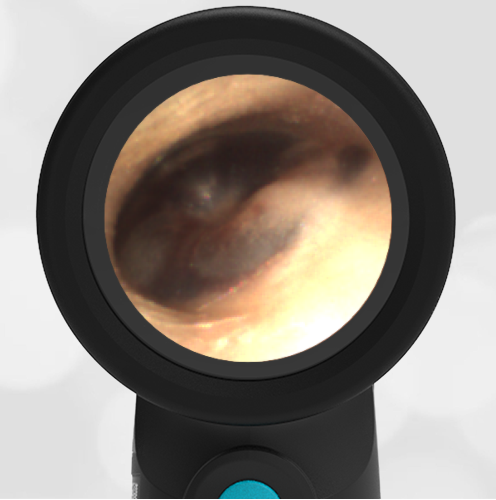
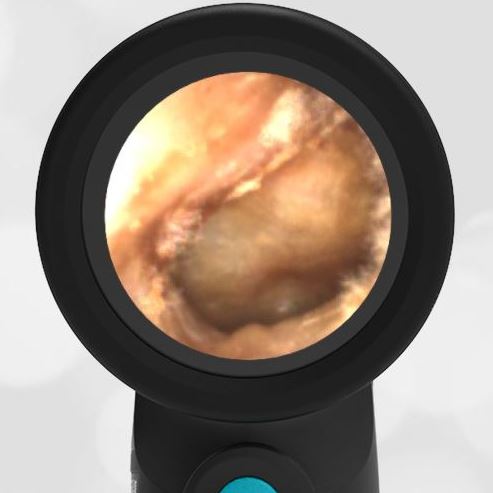
In the ED, the child was afebrile and well-appearing. However, when approached for the otoscopic examination, she immediately started to cry and became extremely upset. Despite being less than cooperative, the Wispr digital otoscope captured the following image of her left tympanic membrane (TM).
What is the next step in the management of this patient?
The child has a middle ear effusion (MEE). No additional management is required.

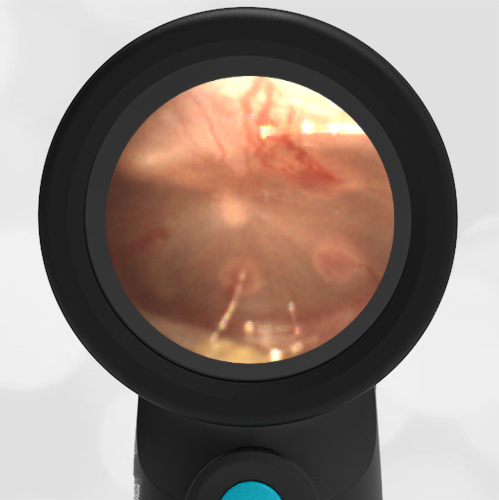
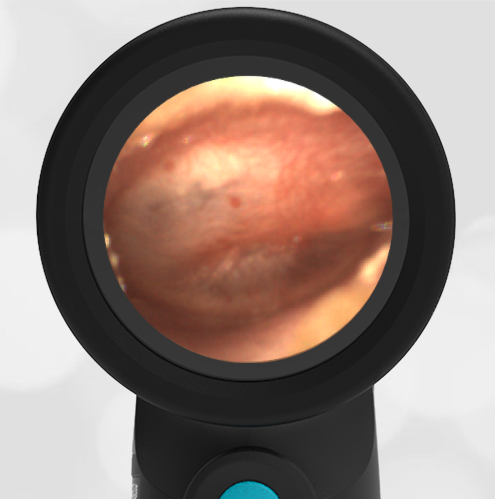
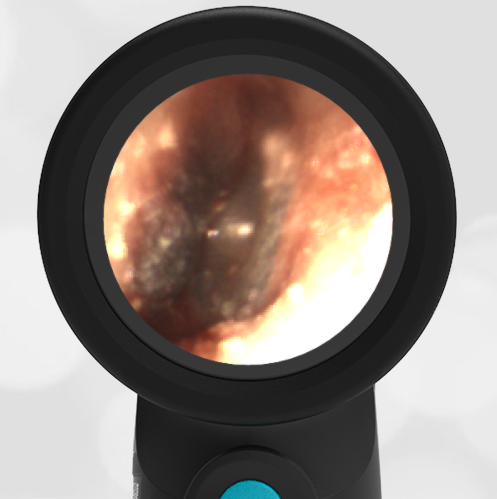
The child’s Wispr exam clearly demonstrates the presence of middle ear fluid, with air-fluid levels noted behind translucent TMs. Even though the fluid appears milky, the TMs are not bulging nor do they appear inflamed with marked injection. In fact, the malleus is prominent which indicates the pars flaccida is retracted, likely due to negative middle ear pressure associated with resolving acute otitis media (AOM). The presence of MEE and the negative pressure may be causing the child to “stick her fingers in her ear” but they do not indicate an acute infection, thus she does not need to be on another course of antibiotics.
Mom expressed concern about the previous antibiotic prescriptions and the challenges encountered during the ear examination. A review of the child’s electronic medical record (EMR) was performed to better understand her medical history. One note provided the medical decision-making for at least one of her prescriptions (paraphrased): “The child was fussy and uncooperative during the ear exam, limited view but TMs seemed red.” It is unknown if the child did indeed have TM bulging at this visit, however, the documented physical findings as well as the child’s challenging exam (which was clearly on display in the ED) do not seem to indicate the need to immediately start antibiotics. Many clinicians will agree that this is an unfortunate and all-too-familiar scenario with regard to identifying the source of fussiness or fever in an uncooperative child. Overcalling AOM due to lack of access to the TM results in unnecessary antibiotics, expense, and worry and can detract from identifying a more serious etiology for the child’s fever. Fortunately, Wispr digital otoscopy is providing clinicians with a tool to address this challenge and improve diagnostic certainty. In this case, the combined otoscopic examination time for both ears lasted ten seconds and allowed the child’s parent and the clinician to be confident in the diagnosis and to avoid another course of unneeded antibiotics.
WiscMed has published a visual guide to the diagnosis of common ear conditions that can be found here.
Here are the complete video exams of the left and right ear. Both demonstrate MEE.
|
Left Ear |
Right Ear |